Real “health care” happens when telemedicine is closely joined to a connected-care delivery model that has prevention and continuity-of-care at its core. This model has been defined well, but only sparsely adopted. As John Hockenberry, host of the morning show “The Takeaway” on National Public Radio, eloquently puts it: “health is not episodic.” We need a continuous care system.

How do we get the “right care to the right patient at the right time”? Schleidgen et al define Precision Medicine also known as Personalized Medicine (1) as seeking “to improve stratification and timing of health care by utilizing biological information and biomarkers on the level of molecular disease pathways, genetics, proteomics as well as metabolomics.” Precision Medicine (2) is an orthogonal, multimodal view of the patient from her/his cells to pathways to organs to health and disease. There are several devices and transducers that would catalyze telemedicine: Radiology, Pathology, and Wearables. I will focus on Radiology for this part of my three-part series, since all of these modalities use multi-spectral imaging.
Where first?
The world is still mostly rural. According to World Bank statistics, 19% of the USA is rural, but the worldwide average is about 30% which is a spectrum from 0% rural (Hong Kong) to 74% rural (Afghanistan). With the recent consolidations (since 2010 in the US) of hospitals into larger organizations (3), it is this 30% to 70% of the world with sparse network connectivity that needs telemedicine sooner than the well-off “worried well” folks who live in dense urban areas with close access to healthcare. China has the world’s largest number of hospitals at around 60,000 followed by India at around 15,000. The US tally is approximately 5,700 hospitals. The counter-argument to the rural needs in the US is the risk of reduction of physician numbers (4), the growing numbers of the urban poor and the elderly. Then there is the plight of poor health amongst the world’s millions of refugees who are usually stuck in no-mans-lands, fleeing conflicts that never seem to wane. All these use-cases are valid, but need prioritization.
Connected Health and the “Saver App”
Many a fortune has been made by devising and selling “killer apps” on mobile platforms. In healthcare what we need is a “saver app.” Using the pyscho-social keys to the success of these “sticky” technologies, Dr. Joseph C. Kvedar succinctly builds the case for connected health in his recent book “The Internet of Healthy Things” with three strategies and three tactics:
Strategies: (1) Make It about Life; (2) Make It Personal; and (3) Reinforce Social Connections.
Tactics: (1) Employ Messaging; (2) Use Unpredictable Rewards; and (3) Use the Sentinel Effect.
Dr. Kvedar calls this “digital therapies.”
The Vendor Neutral Archive (VNA) and Virtual Radiology
The Western Roentgen Society, a predecessor of the Radiological Society of North America (RSNA), was founded in 1915 in St. Louis, Missouri (soon after the invention of the X-Ray tube in Bavaria in 1895). An interactive timeline of Radiology events can be seen here. Innovations in Radiology have always accelerated the innovations in healthcare.
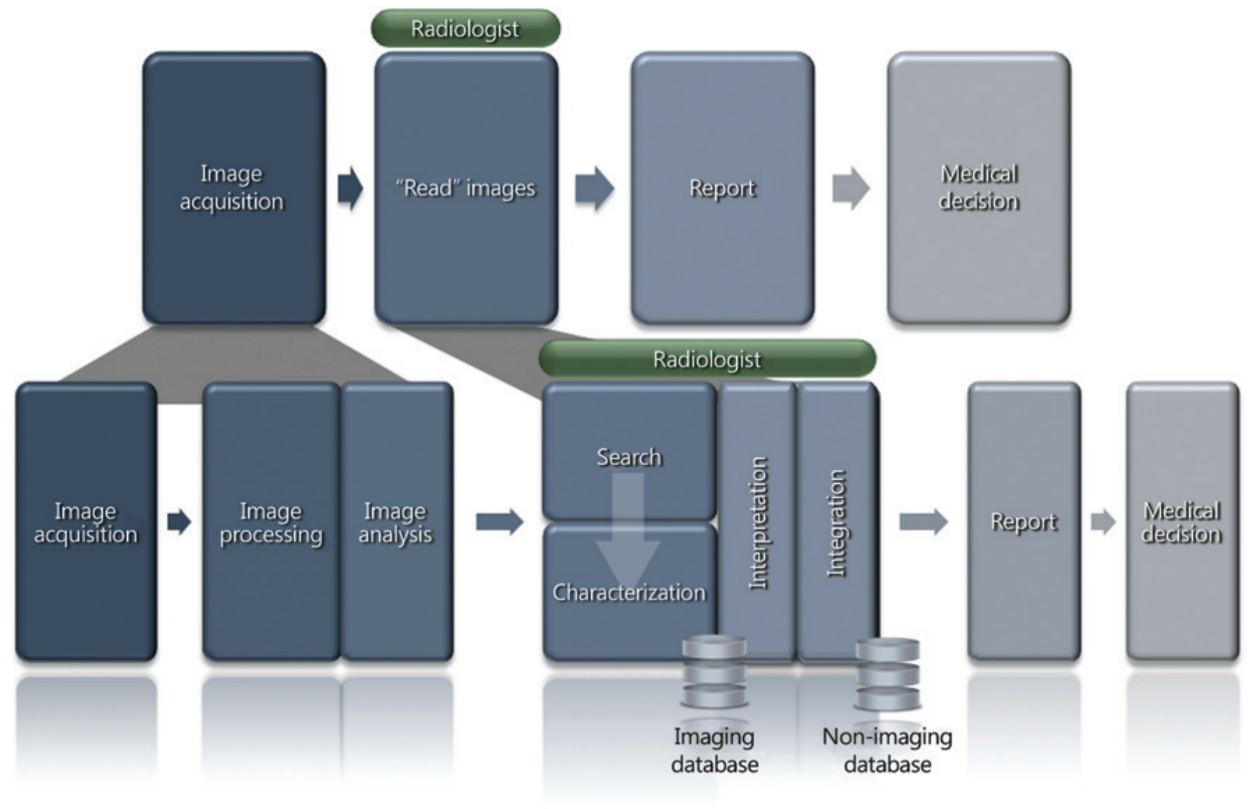
The Radiology value chain is in its images and clinical reporting, as summarized in the diagram below (5):
To scale this value-chain for telemedicine, we need much larger adoption of VNA, which is an “Enterprise Class” data management system. A VNA consolidates multiple Imaging Departments into:
- a directory,
- associated storage and
- lifecycle management of data
The difference between PACS (Picture Archiving and Communications System) (6) and VNA is the Image Display and the Image Manager layers respectively.
The Image Display layer is a PACS Vendor or a Cloud based “image program”. All Admit, Discharge and Transfer (ADT) information must reside with the image. This means DICOM standards and HL7 X.12N interoperability (using service protocols like FHIR) are critical. The Image Manager for VNA is the “storage layer of images”, either local or cloud based. For telemedicine to be successful, VNA must “scale-out” exponentially and in a distributed manner within a privacy and security context.
VNA’s largest players (alphabetically) are: Agfa, CareStream, FujiFilm (TeraMedica), IBM (Merge), Perceptive Software (Acuo), Philips and Siemens. The merger of NightHawk Radiology with vRad which was then acquired by MedNax and IBM’s acquisition of Merge Healthcare (in Aug 2015) are important landmarks in this trend.
One of the most interesting journal articles in 2015 was on “Imaging Genomics” (or Radiomics) of glioblastoma, a brain cancer. By bidirectionally linking imaging features to the underlying molecular features, the authors (7) have created a new field of non-invasive genomic biomarkers.
Imagine this “virtual connected hive” of patients on one side and physicians, radiologists and pathologists on the other, constantly monitoring and improving the care of a population in health and disease at the individual and personal level. Telemedicine needs to be the anchor architecture for Precision Medicine. Without Telemedicine (and VNA), there is no Precision Medicine.
Postscript: Telepresence in mythology
Let me end this tale of distance and care with a little echo from my namesake, Sanjaya, who is mentioned in the first chapter of the first verse of the Bhagvad Gita (literally translated as the “Song of the Lord”) – an existential dialog between the warrior Arjuna and his charioteer, Krishna. The Gita, as it is commonly known, is set within the longest Big Data poem with over 100,000 verses (and 1.8 million words), the Mahabharata, estimated to be first written around 400 BCE.
Dhritarashtra, the blind king, starts this great book-within-book by enquiring: “O Sanjaya, what did my sons and the sons of Pandu decide about battle after assembling at the holy land of righteousness Kurukshetra?”
Sanjaya starts the Gita by peering into the great yonder. He is bestowed with the divine gift of seeing events afar (divya-drishti); he is the king’s tele-vision – and Dhritarashtra’s advisor and charioteer (just like Krishna in the Gita). The other great religions and mythologies also mention telepresence in their seminal books.
My tagline for the “trickle down” in technology innovation flow is “from Defense to Life Sciences to Pornography to Finance to Commerce to Healthcare.” One interpretation of the Mahabharata is that it did not have any gods – all miracles were added later. Perhaps we have now reached the pivot point for telepresence which has happened in war to “trickle down” into population scale healthcare without divine intervention or miracles!
References:
- Schleidgen et al, “What is personalized medicine: sharpening a vague term based on a systematic literature review”, BMC Medical Ethics, Dec 2013, 14:55
- “Toward Precision Medicine”, Natl. Acad. Press, June 2012
- McCue MJ, et al, “Hospital Acquisitions Before Healthcare Reform”, Journal of Healthcare Management, 2015 May-Jun; 60(3):186-203.
- Petterson SM, et al, “Estimating the residency expansion required to avoid projected primary care physician shortages by 2035”, Annals of Family Medicine 2015 Mar; 13(2):107-14. doi: 10.1370/afm.1760
- Enzmann DR, “Radiology’s Value Chain”, Radiology: Volume 263: Number 1, April 2012, pp 243-252
- Huang HK, “PACS and Imaging Informatics: Basic Principles and Applications”, Wiley-Blackwell; 2 edition (January 12, 2010)
- Moton S, et al, “Imaging genomics of glioblastoma: biology, biomarkers, and breakthroughs”, Topics in Magnetic Resonance Imaging. 2015