This post is co-authored by Youssef Serghat, a Solution Architect at Dell Digital Business Services
Paving the way for an integrated and coordinated Health Information Exchange system following the VA model
When it comes to quality, cost-effective and evidence-based treatments, U.S. Veteran’s Administration (VA) healthcare system rarely comes to the mind of most Americans. In his book “Best Care Anywhere,” Phillip Longman describes why VA, contrary to the public perception, today is considered the safest, most effective and integrated healthcare delivery system in the world.
Veterans Health Information Systems and Technology Architecture (VistA), is a bundle of thousands of programs that were collaboratively developed and integrated by doctors and programmers in VA healthcare facilities across the country. Today, VistA is open source software, considered the most comprehensive Electronic Health Records (EHR) application in the U.S., and embraced by many countries around the world. What makes VistA effective is its obsession on delivering the best-value care, with a focus on long-term patient care. This focus prevents medical errors and follows a best-in-class model for medical studies. VistA accomplishes this coordinated care through interoperability and the use of its unique and highly integrated EHR system.
The successes realized by the VA integrated IT model were objectives of the Health Information Exchange (HIE) initiatives. However, these HIEs came short in creating a truly integrated and interoperable electronic health information exchange that is focused on improving efficiency and cost in both the delivery process and patient outcomes. The complexity of HL7 standards and failure to use EHR systems in a more meaningful way are two main factors for HIEs shortcomings.
New government incentives and Meaningful Use requirements, along with HL7 FHIR standards and open source technology are designed to support the creation of a truly integrated Health Information Exchange (HIE) ecosystem that follows the VA healthcare model.
Meaningful Use
Meaningful Use (MU) is one of the key features of the Health Information Technology for Economic and Clinical Health (HITECH), which is part of American Recovery and Reinvestment Act (ARRA), passed by the U.S. Congress and signed into law by President Obama in 2009. The goal of MU is to encourage the use of EHRs in a more meaningful, coordinated and integrated way. In their book “Hacking Healthcare,” Fred Trotter and David Uhlman describe MU as “an attempt by the U.S. government to define the baseline for what a clinician using EHR should be able to accomplish.” They also describe how Meaningful Use will be “at the heart of healthcare reform in the United States for the next several decades.”
Before the creation of Meaningful Use requirements, the VA healthcare system accomplished most of the goals set in the three stages of Meaningful Use using its common integrated EHR system, coordinated and shared among all VA facilities around the world. Hospitals within the digitized VA system can deliver more services because their common digital records allow doctors and clinics to better-coordinate complex treatment regimens throughout the life of their patients
Open API-driven FHIR redefines interoperability and integration
There are more than 1000 certified EHR systems in production today, most of them proprietary. Developed over the last 20 years, these EHR systems have been — and are — supporting a number of HL7 standards including V2, V3 and CDA. However, these standards are complex and difficult to integrate. A broader and widely accepted, simple yet powerful standard was required to address the fast growing need for seamless information flow in the healthcare ecosystem. Fast Healthcare Interoperability Resources (FHIR) is the new HL7 that is intended to address this gap and simplify health information exchange. FHIR considers implement-ability as its most fundamental precept. It defines a flexible framework for interoperability, and leverages open source development and common web technologies including HTTP, REST, XML and JSON and simplify healthcare information exchange
FHIR enables a granular way to exchange data by using RESTful style approach. FHIR solutions are built from a set of modular components called “Resources.” Data Access Framework (DAF) leverages HL7 FHIR, C-CDA and existing IHE standards to standardize access to Meaningful Use data located in EHR or in other systems of records.
FHIR is simple, easy to understand, easy to implement and has wider applicability than all the standards that we had in Healthcare so far for integration and interoperability needs. FHIR is expected to help providers achieve meaningful use in a more efficient manner. FHIR and REST APIs are actually much beyond enabling interoperability; they are also expected to revolutionize healthcare ecosystem by fueling innovation and digital health and enabling creation of “smart apps.”
An implementation approach
An important and major step in the FHIR and REST APIs implementation process to support HIE is the data mapping from the EHR and other systems of record. It’s important to select tools or implement generic and extensible mapping interfaces and avoid being locked in a proprietary or rigid framework in this step.
FHIR is not a security protocol, and it does not define any security related functionality. OAuth is well recognized open standards for authentication and can be integrated to support security access to FHIR RESTful APIs.
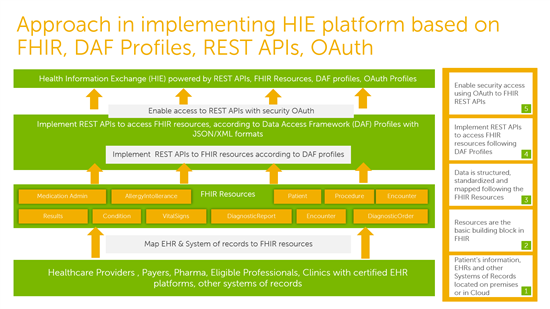
Figure 1, shows steps involved in implementing FHIR RESTful APIs based on DAF Profiles and OAuth for supporting Health Information Exchange.
Armed with HL7 FHIR standards, DAF Profiles, RESTful APIs, and other open source technology, organizations can join an ecosystem that supports standard Health Information Exchange, adapts to the implementation of Meaningful Use, and facilitates the creation of clinical and smart apps.
Figure 2: Health Information Exchange powered by FHIR, DAF standards and open source technology
A moving target
The success of the VA healthcare model is the result of its continued focus on implementing efficiency in the delivery process and improving patient outcomes through coordination and the use of its integrated EHR system.
Meeting Meaningful Use (MU) regulations requires digital innovation in data interoperability, security and accelerated time-to-value. MU is a moving target, and its requirements will keep evolving to improve medical care, reduce cost and create opportunities that can only be possible when healthcare providers, researchers, clinics and patients can share data easily. In his book The Creative Destruction of Medicine, How the digital revolution will create better healthcare Dr. Eric Topol describes how “Medicine is about to go through its biggest shakeup in history.” Dr. Topol lays out a vision for how technologies, including wireless sensors, genomics, imaging, health information systems, the Internet and social networks, will converge to create new, individualized medicine. MU will certainly evolve with this new individualized medicine. The integrated healthcare system will increasingly become a cornerstone of healthcare delivery transformation driven by information and digital technologies. To achieve a truly integrated healthcare, FHIR and open APIs are a critical next step.
 About the co-author
About the co-author
Youssef Serghat is a Solution Architect at Dell Digital Business Services. He has led and contributed to a number of enterprise and cloud integration solutions supporting customers in telecommunication, airline, e-commerce, aerospace and healthcare industries. He started his 20 years IT career when CORBA was the standard and the facto in enterprise integration and today he is using SOA, ESB, and APIs, to solve enterprise and cloud integration unique challenges.